Protecting PHI: incidental disclosure hipaa Essentials for Clinicians
Understand incidental disclosure hipaa and how it differs from a breach, plus practical steps to safeguard PHI and your practice.

An incidental disclosure under HIPAA is one of those concepts that sounds complicated but is actually pretty intuitive. At its core, it's a secondary, unavoidable exposure of Protected Health Information (PHI) that happens while you're doing something you're already allowed to do—as long as you've taken reasonable steps to prevent it.
Think of it as unavoidable collateral exposure. It's not a violation because it happens despite your best efforts to protect patient privacy.
Demystifying Incidental Disclosures

Here’s a classic real-world example: imagine two nurses having a quiet, necessary conversation about a patient's care plan in a hospital hallway. They're speaking softly and being discreet, but a visitor walking by happens to overhear the patient's name. That brief, unintentional exposure is a perfect example of an incidental disclosure HIPAA allows for.
This is a critical distinction because not every accidental reveal of PHI is a reportable breach. The HIPAA Privacy Rule is practical; it acknowledges that it’s impossible to create a completely sterile, risk-free environment in a busy healthcare setting. Understanding this separates a minor, permissible event from a serious compliance failure.
The Two Pillars of Permissibility
For an accidental exposure to truly count as incidental and not a violation, it has to be supported by two foundational pillars established by HIPAA. These principles are how you demonstrate that you’ve done your due diligence in protecting sensitive information.
Reasonable Safeguards: This is all about the practical, common-sense measures you have in place to protect PHI. Think things like installing privacy screens on computers at the check-in desk, speaking in lowered voices when discussing patient matters, or making sure sensitive documents aren't just left sitting out in public view.
Minimum Necessary Standard: This rule is simple but powerful: you should only use, disclose, or request the absolute minimum amount of PHI needed to get the job done. For example, a waiting room sign-in sheet should only ask for a patient's name, not their diagnosis or medical history.
This framework is essential for everyone on your team. It applies just as much to clinical staff handling patient charts as it does to marketing teams using online forms to capture inquiries from potential new patients. When you collect any data, it’s vital that your tools and processes align with these privacy principles. A robust privacy policy is the bedrock that supports all of these safeguards.
Why This Distinction Matters
Getting this right isn't just about compliance—it directly impacts your daily operations. When your team can confidently identify the difference between an incidental disclosure and a true breach, they can do their jobs effectively without constantly fearing they'll violate the law for minor, unavoidable exposures.
An incidental disclosure isn't a "free pass." It's an acknowledgment by HIPAA that perfect privacy is unattainable. The real focus is on demonstrating a consistent, reasonable effort to protect patient information at all times.
This understanding allows you to focus your time and resources where they matter most: on preventing the genuine, negligent breaches that come with severe penalties. By implementing thoughtful safeguards and sticking to the minimum necessary standard, you create a culture where patient privacy is respected, and incidental exposures remain just that—incidental. That proactive approach is the heart of a strong HIPAA compliance program.
The Critical Line Between a Disclosure and a Breach
Navigating HIPAA compliance often feels like walking a tightrope. One wrong step can turn an acceptable, everyday interaction into a serious violation. Understanding the fine line between a permissible incidental disclosure and a reportable HIPAA breach isn't just a legal checkbox—it's a core part of protecting patients and your organization.
The real difference comes down to intent and foresight. It’s the difference between a private conversation being accidentally overheard versus shouting sensitive information across a crowded waiting room. A disclosure becomes a breach when common-sense precautions are ignored.
Drawing the Line with Real-World Scenarios
To make this crystal clear, let's look at two scenarios that happen all the time.
First, imagine a doctor and a nurse discussing a patient's new medication in a semi-private alcove of a busy hospital hallway. They're speaking quietly, but a visitor walking past happens to overhear the patient's last name. This is a classic incidental disclosure. The main purpose of the conversation was patient care, and they took reasonable steps (speaking quietly in a less-trafficked spot) to protect privacy.
Now, flip the script. A medical assistant leaves a patient's full chart, wide open, on the reception counter while they take a lunch break. Anyone in the waiting room can easily see the patient’s name, diagnosis, and treatment plan. This is a breach, plain and simple. It was caused by a failure to use a basic, reasonable safeguard—in this case, just closing the file or putting it away.
That dividing wall between the two is the presence of those safeguards. One demonstrates due diligence; the other shows negligence.
Why Reasonable Safeguards Are Everything
"Reasonable safeguards" are the practical, proactive steps you take to protect Protected Health Information (PHI). They don't have to be foolproof or eliminate every conceivable risk, but they must be appropriate for your specific environment.
Under HIPAA, incidental disclosures are permissible only if you've implemented these safeguards and are following the minimum necessary standard. These are the secondary, often unavoidable exposures that happen during a legitimate, necessary activity—like calling a patient's name in a waiting room or a colleague catching a glimpse of a name on your screen as they walk past your desk.
As communication has moved online, these safeguards are more critical than ever. It's vital to understand why overlooking HIPAA and PHI in video conferencing could put your business at risk and to apply the same principles of care to digital interactions.
Incidental Disclosure vs HIPAA Breach At a Glance
Sometimes, seeing the key differences side-by-side makes the distinction click. This table breaks down what separates a permissible, accidental exposure from a reportable violation.
| Characteristic | Incidental Disclosure (Permissible) | HIPAA Breach (Impermissible) |
|---|---|---|
| Nature of Exposure | Secondary byproduct of a permitted activity; unavoidable despite safeguards. | Direct result of negligence or a failure to implement proper safeguards. |
| Safeguards | Reasonable safeguards were in place to minimize the exposure. | Reasonable safeguards were absent, ignored, or inadequate. |
| Intent | Unintentional and accidental. | Often preventable and may involve negligence or willful disregard for policy. |
| Consequences | No formal reporting required; documented internally as a best practice. | Requires formal notification to the patient and HHS, potential fines, and corrective action. |
Ultimately, it's your proactive security posture that defines which side of the line you're on.
Your commitment to protecting data—from the physical layout of your office to the digital security of your patient intake forms—is what truly matters. This is where having the right policies and tools makes all the difference. To see how modern platforms handle this, you can review a breakdown of comprehensive security measures for data protection designed to meet today's compliance standards.
Recognizing Incidental Disclosures in Your Daily Workflow
Understanding the textbook definition of an incidental disclosure is one thing. Spotting one in the middle of a busy workday is a completely different ballgame.
The truth is, these small exposures aren't rare events; they happen in countless ways every single day. The first step toward making sure your safeguards are actually working is learning to recognize these moments for what they are.
From the front desk check-in to the chatter outside an exam room, opportunities for minor, permissible disclosures are literally everywhere. The real skill is knowing where the line is between an unavoidable slip and a preventable accident.
Take the classic patient sign-in sheet at reception. It's a necessary part of the workflow, but it’s almost guaranteed that one patient will catch a glimpse of the name above theirs. This is a textbook incidental disclosure. But what happens if that same sheet has a column for "Reason for Visit"? Now you're collecting more than the minimum necessary information, and a casual glance goes from incidental to a potential violation. It’s this constant, real-time assessment that builds a true culture of compliance.
Common Examples in Physical and Digital Spaces
Incidental disclosures aren’t just about paper records or conversations in the hallway. As healthcare moves online, the risks multiply, and your team needs to be just as sharp about digital workflows as they are about physical ones.
Here are a few scenarios where a minor disclosure is likely permissible, assuming you’ve got those reasonable safeguards in place:
- Waiting Room Chatter: A nurse calls out a patient's first name and last initial. Someone else in the waiting room overhears it.
- The Pharmacy Counter: A pharmacist has a quiet, brief chat with a patient about their prescription, and the person next in line catches a few words.
- A Telehealth Call: During a video appointment, a family member quickly walks through the background of the patient's room, unintentionally seeing the provider on screen.
This decision tree helps visualize how an accidental exposure either stays a permissible disclosure or becomes a reportable breach, with safeguards being the deciding factor.
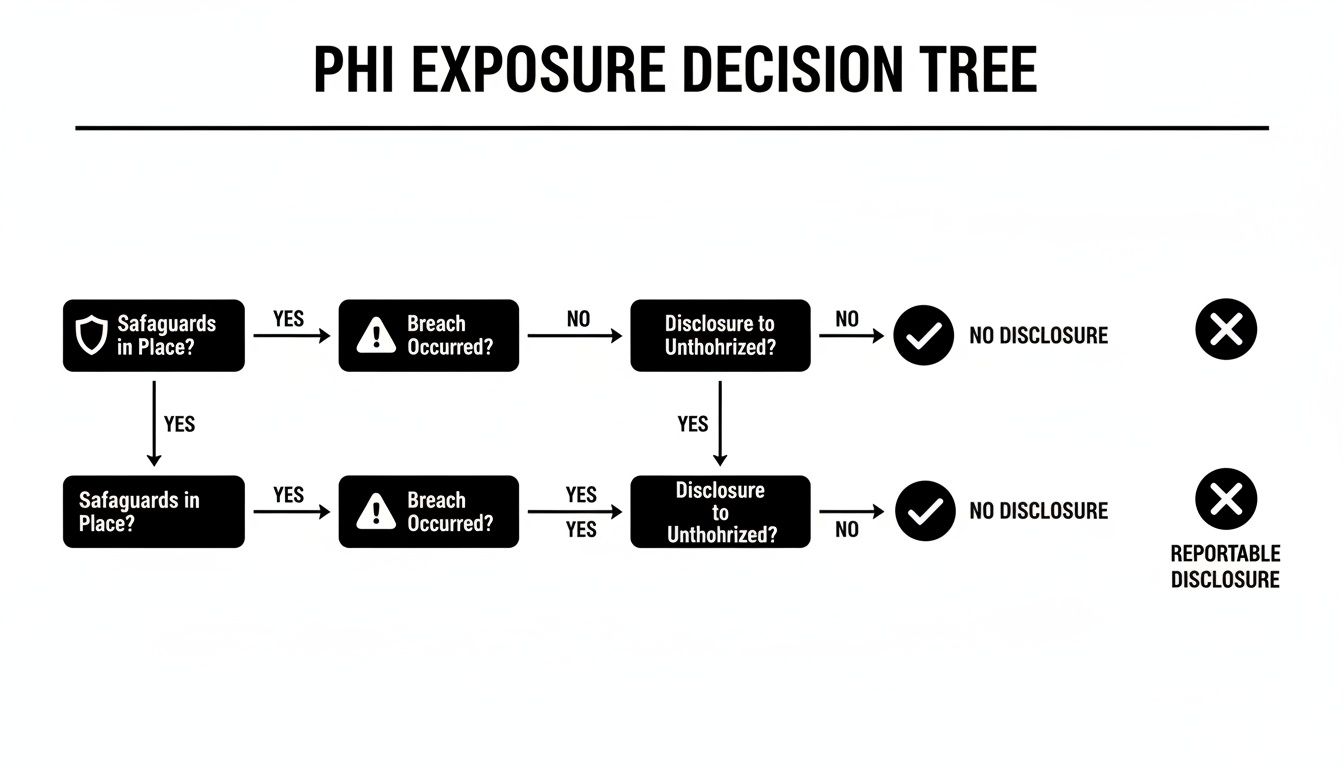
If there’s one thing to take away from this flow, it's that having reasonable safeguards in place is what stops a simple accident from turning into a compliance nightmare.
The Growing Risk in Digital Communications
These days, a patient’s journey often starts online, usually with a contact or appointment request form on your website. This digital front door is a massive, and often overlooked, area of risk.
Think about it: an unsecured web form that emails patient questions to a shared inbox is just waiting for an unauthorized person to see it. An automated email reply that helpfully includes the sensitive health details they just submitted could easily be intercepted or sent to the wrong address by mistake.
These situations are exactly why your choice of software and tools matters so much. Using HIPAA-compliant platforms for collecting patient data isn't just a "nice-to-have"—it's a foundational safeguard. For a closer look at locking down these digital entry points, check out our guide on best practices for secure form creation.
The core principle is the same, whether you're dealing with a clipboard or a web form: you are responsible for putting reasonable measures in place to protect PHI. An incidental disclosure is only okay when it's the unavoidable byproduct of a necessary task that was otherwise done securely.
These aren't just theoretical worries. In 2023, unauthorized access and disclosure of PHI accounted for 14.83% of all reported breaches on the OCR’s portal. Cases like the $80,000 settlement against St. Joseph's Medical Center for accidentally sharing patient information with a reporter show just how easily this can happen—and that these incidents often reveal systemic problems, not just one-off mistakes. Vigilance isn't optional.
How to Implement Reasonable Safeguards That Actually Work
Knowing what an incidental disclosure is under HIPAA is one thing. Actually stopping one from spiraling into a full-blown breach is another. This is where theory meets reality. Your goal is to build a strong framework of reasonable safeguards—the tangible, everyday actions that protect patient data.
These aren't just abstract legal ideas. They're the practical steps you weave into your team's workflow, your office layout, and your technology.

A solid prevention strategy needs layers. You have to think about how your team behaves, how your physical space is set up, and how your software guards information. By focusing on these three core areas—administrative, physical, and technical—you create a defense system that makes privacy the default, not an afterthought.
Administrative Safeguards: The Foundation of Your Defense
Think of administrative safeguards as the "rules of the road" for data privacy in your organization. These are the policies, procedures, and training that form the backbone of your entire compliance strategy. This is where you set clear expectations and give your team the knowledge to handle Protected Health Information (PHI) responsibly.
Key administrative controls look like this:
- Comprehensive Staff Training: Forget the once-a-year slideshow. Your training needs to be regular and scenario-based, teaching employees to spot disclosure risks specific to their jobs. A front-desk employee faces completely different risks than a clinician or a marketer.
- Clear Privacy Policies: Develop and hand out straightforward policies that spell out how to handle PHI. This needs to cover everything from verbal conversations and shredding documents to using personal cell phones for work.
- Designated Privacy Officer: You need one person who owns HIPAA compliance. This individual is responsible for overseeing the rules, answering staff questions, and investigating any potential incidents.
Physical Safeguards: Securing Your Environment
Next up are the physical safeguards. These are all about the tangible environment where your team works and your patients visit. The goal here is simple: minimize the chance that PHI can be seen or heard by the wrong people. It mostly comes down to common-sense adjustments to your workspace.
Consider putting these physical measures in place:
- Optimized Office Layout: Arrange waiting rooms, reception desks, and workstations to boost privacy. Make sure conversations at the check-in counter can’t be easily overheard by everyone sitting nearby.
- Privacy Screens: This is a cheap and easy win. Install privacy filters on any computer monitor in a public-facing or high-traffic area to stop "shoulder surfing."
- Secure Document Storage: Use locked file cabinets for paper records. A "clean desk" policy is also crucial to make sure sensitive documents aren't just left sitting out.
The most effective safeguards are often the simplest. Lowering voices, turning a computer screen away from public view, or moving a sensitive conversation to a private room are no-cost actions that significantly reduce the risk of an incidental disclosure.
These physical and administrative controls are two sides of the same coin. The best training in the world won't matter if an employee is working on an exposed computer screen in a busy reception area. It's the combination of smart policy and a secure physical space that creates a truly resilient defense. To make sure all your digital communications, including faxes, are secure, it's worth reviewing a guide on HIPAA compliant internet fax for extra security protocols.
Technical Safeguards: Protecting Your Digital Front Door
Finally, we have technical safeguards. These are the technology-based controls that protect electronic PHI (ePHI), and in today's world, this is where the biggest risks live. Your website forms, email, and patient portals are all potential weak spots if they aren't locked down.
This is especially true for your lead capture and patient intake forms. They're often the very first place you collect sensitive data, and using a standard, non-compliant form builder is like leaving your digital front door wide open. A single misconfiguration could expose thousands of patient records, which is why choosing a HIPAA-compliant tool is non-negotiable.
Here’s where modern, purpose-built platforms make a huge difference:
- Orbit AI: Built from the ground up with security in mind, Orbit AI provides end-to-end encryption for all form submissions. This ensures PHI is protected the moment it’s entered. Its AI qualification engine also helps enforce the "minimum necessary" rule by only asking for detailed health information after a user is identified as a legitimate prospect, cutting down on unnecessary data collection.
- HIPAA-Compliant Email: When you're emailing PHI to patients or other providers, you have to use an encrypted email service. Standard email is not secure and can be easily intercepted.
- Access Controls: Every system containing ePHI needs unique user logins. Access should be granted strictly on a need-to-know basis, limiting what each team member can see based on their role.
At the end of the day, your technical safeguards must be just as strong as your physical and administrative ones. For any organization relying on online forms to grow, digging into the details of form security and data protection is a critical step toward building a truly comprehensive compliance program.
Your Action Plan for Handling Incidental Disclosures
Even with the best privacy controls in place, accidental exposures are a fact of life. When one happens, a clear, pre-defined action plan is your best defense against panic, missteps, and non-compliance. Your team shouldn't be scrambling with uncertainty; they need a straightforward protocol to follow.
This simple, three-step framework—Assess, Document, and Review—is designed to do just that. It transforms a moment of potential risk into a structured, compliant response, ensuring every incident is handled consistently and correctly. More importantly, it turns these small events into opportunities to strengthen your overall privacy posture.
Step 1: Assess the Situation Immediately
The second a potential incidental disclosure is spotted, the first move is a rapid, calm assessment. The goal isn't to assign blame, but to figure out if the event meets the criteria for a permissible disclosure or if it has crossed the line into a reportable breach.
You need to ask three critical questions right away:
- Were reasonable safeguards in place? For example, was a conversation held in a low voice, or was a privacy screen used on the computer monitor?
- Was the minimum necessary standard followed? Did the exposure involve only the absolute essential amount of Protected Health Information (PHI)?
- Was the disclosure a byproduct of a permitted activity? Did it happen while a staff member was performing a necessary job function, like patient care or scheduling?
If you can confidently answer "yes" to these questions, the event is almost certainly a permissible incidental disclosure. If those safeguards were missing or flat-out ignored, you have to escalate the issue immediately and kick off your formal breach notification process.
Step 2: Document Everything
Let’s be clear: documentation isn't optional. It’s your proof of due diligence. Keeping a detailed internal log of every potential disclosure—even the minor ones that are definitely not breaches—is a critical best practice. This log shows auditors and regulators that you take privacy seriously and have a real process for managing these incidents.
Your documentation for each event should include:
- The date and time it happened.
- A brief, factual description of the incident.
- The specific PHI that was potentially exposed.
- The individuals involved (staff, patients, any third parties).
- The immediate actions taken to mitigate any risk.
- Your final call on whether it was an incidental disclosure HIPAA allows or a breach.
Documenting every single event, no matter how small, creates a valuable data trail. It helps you spot recurring issues or weak spots in your safeguards, allowing you to make targeted improvements before a minor slip-up turns into a major breach.
This level of diligence has never been more important. In 2023, healthcare data breaches hit shocking new levels, with 725 breaches reported to the Office for Civil Rights and over 133 million patient records exposed. The sheer volume of these incidents is exactly why regulators scrutinize every organization's ability to manage and document its privacy practices. You can learn more about the latest trends in the most recent healthcare data breach statistics.
Step 3: Review and Refine Your Safeguards
The final step is to treat every incident as a learning opportunity. A single incidental disclosure might just be a one-off fluke, but a pattern of similar incidents points to a systemic weakness that you need to fix.
Review your disclosure log on a regular basis to look for trends. Are a lot of disclosures happening at the front desk? Maybe it's time to rearrange the physical layout or install a sound-masking system. Are mistakes happening with your digital forms? That’s a clear signal to audit your technology and processes. For some guidance on optimizing your digital intake, you can always get in touch with our support team for best practices.
By using this Assess, Document, and Review cycle, you build a resilient compliance culture. You’ll shift from just reacting to incidents to proactively strengthening your defenses, making sure that patient privacy stays at the very core of your operations.
Common Questions About Incidental Disclosures
Navigating the day-to-day realities of patient privacy means you're going to have specific, practical questions. It’s unavoidable. This final section tackles some of the most common uncertainties healthcare professionals and their business associates run into when dealing with an incidental disclosure under HIPAA.
Think of this as your rapid-response guide for the real-world scenarios that pop up in waiting rooms, during phone calls, and on your website. Getting these answers right reinforces the core principles we've discussed and helps build a stronger, more resilient compliance culture from the ground up.
Is Calling a Patient's Name in a Waiting Room a HIPAA Violation?
No, this is a classic example of a permissible incidental disclosure HIPAA allows for. The Privacy Rule is practical; it recognizes that calling a patient's name is a necessary part of healthcare operations. The key, as always, is sticking to the minimum necessary standard.
To stay compliant, your staff should only announce the patient's name. They absolutely should not include sensitive details like the reason for the visit or the specific doctor they are seeing. For an extra layer of protection in a busy clinic, just using a first name and last initial is a simple, highly effective safeguard.
How Does the Minimum Necessary Rule Apply to Online Forms?
The Minimum Necessary Rule is absolutely critical for your digital front door—especially your patient intake and lead capture forms. The rule dictates that you should only collect the data strictly required for the specific purpose of that form, at that specific stage.
A simple newsletter signup form, for example, should only ask for an email address. A more involved appointment request might reasonably need a name and phone number. You have to resist the temptation to capture detailed medical history or other sensitive PHI unless it is critical for that immediate step.
This is where smart, secure form tools become invaluable, helping you enforce this rule automatically.
A well-designed form can use conditional logic to wait and ask for more detailed PHI after a user has been qualified or has explicitly consented to move forward. This design minimizes data exposure at every stage of the patient journey.
What Is the First Step to Better Manage Incidental Disclosures?
The single most effective first step is to conduct a thorough and honest risk assessment. You simply can't protect against risks you haven't identified. This means systematically reviewing every point in your workflow—both physical and digital—where Protected Health Information is handled.
Your assessment should map out potential weak spots in areas like:
- Physical Environment: Your office layout, the setup of your reception desk, and where patient charts are stored.
- Communication Protocols: How your team handles phone calls, voicemails, and conversations in shared spaces.
- Digital Touchpoints: A deep dive into your website's contact forms, patient portals, and any third-party software used for scheduling or intake.
Once you have this clear map, you can implement targeted safeguards, update your policies, and train your team on the specific scenarios they're most likely to face. For many practices, securing those digital entry points is the most impactful first move you can make.
Do We Need to Report Every Incidental Disclosure?
No, you are not required to report permissible incidental disclosures to the Office for Civil Rights (OCR). By definition, they are not considered breaches, as long as you've implemented reasonable safeguards and followed the minimum necessary rule.
However, it's a critical best practice to maintain a detailed internal log of these events. This documentation serves as crucial evidence of your due diligence and proves to auditors that you have a proactive process for managing privacy. More importantly, this log helps you spot patterns. A series of similar incidents might reveal a weakness in your safeguards that needs to be fixed before it leads to a real breach.
If your internal review determines that an exposure was not incidental and does in fact constitute a breach, you must then follow the official HIPAA Breach Notification Rule, which includes notifying the affected individuals and the HHS.
Your digital forms are one of the most significant risk areas for PHI exposure. Orbit AI helps you turn this vulnerability into a strength with HIPAA-compliant, AI-powered forms designed to securely capture and qualify leads while protecting patient data at every step. Learn how to build smarter, safer forms at https://orbitforms.ai.
Ready to get started?
Join thousands of teams building better forms with Orbit AI.
Start building for free